- What exactly is a cataract?
- Are there different types of cataracts?
- What causes cataracts? Are they inherited?
- Are cataracts dangerous to the eye?
- What symptoms do people experience with cataracts?
- Can children get cataracts?
- How are cataracts detected?
- Do cataracts affect both eyes?
- Is a cataract the same as macular degeneration or glaucoma?
- Can cataracts be prevented?
- Can cataracts be treated besides having surgery?
- If I have to have cataract surgery, what can I expect during the operation and afterwards?
- What does “no-stitch, no needle” cataract surgery mean?
- What are the current methods of cataract surgery? Is there such a thing as “laser” removal of cataracts?
- What exactly is a lens implant? Is it the same thing as an eye transplant?
- Are there any risks or complications of having cataract surgery?
What exactly is a cataract?
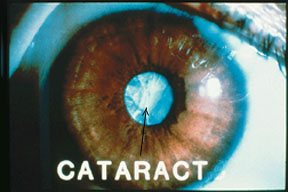
 This usually occurs as a normal part of the aging process of the eye. Many times, the loss oftransparency of the lens is so mild, vision is hardly impaired. When the lens gets cloudy enough to obstruct your vision, it is then called a cataract. Cataract disease is the single greatest cause of blindness world wide. It accounts for over 50% of all blindness, and it affects over 17,000,000 people. Depending upon who you read, between 12 – 50% of all persons over the age of 65 have some form of cataract development.
This usually occurs as a normal part of the aging process of the eye. Many times, the loss oftransparency of the lens is so mild, vision is hardly impaired. When the lens gets cloudy enough to obstruct your vision, it is then called a cataract. Cataract disease is the single greatest cause of blindness world wide. It accounts for over 50% of all blindness, and it affects over 17,000,000 people. Depending upon who you read, between 12 – 50% of all persons over the age of 65 have some form of cataract development.Are there different types of cataracts?
What causes cataracts? Are they inherited?
Are cataracts dangerous to the eye?
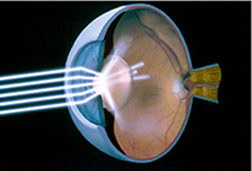
 The eye works very similarly to a camera (See the Eye Anatomy page for details). Light rays travel through the eye and are focused by the cornea and lens onto the surface of the retina which acts like film inside of a camera. When the lens becomes cloudy, depending upon the degree and type of cloudiness, the vision can become impaired in several ways. The typical symptom of cataract formation is blurred vision which frequently is very slow, progressive, and painless. Glare at night and halos around lights are frequently experienced as well. One may notice that colors have become washed out, or that images have taken on a yellowish cast. Many persons experience frequent eyeglasses changes. Double vision is occasionally experienced. There are some situations where distancevision actually improves with cataract development. This is frequently called “second sight.” This occurs when farsighted persons experience improved distance vision with less dependency upon their glasses. This effect from cataract development however is usually only temporary.
The eye works very similarly to a camera (See the Eye Anatomy page for details). Light rays travel through the eye and are focused by the cornea and lens onto the surface of the retina which acts like film inside of a camera. When the lens becomes cloudy, depending upon the degree and type of cloudiness, the vision can become impaired in several ways. The typical symptom of cataract formation is blurred vision which frequently is very slow, progressive, and painless. Glare at night and halos around lights are frequently experienced as well. One may notice that colors have become washed out, or that images have taken on a yellowish cast. Many persons experience frequent eyeglasses changes. Double vision is occasionally experienced. There are some situations where distancevision actually improves with cataract development. This is frequently called “second sight.” This occurs when farsighted persons experience improved distance vision with less dependency upon their glasses. This effect from cataract development however is usually only temporary.Can children get cataracts?
How are cataracts detected?
 Many of the symptoms of cataract development can occur with other ocular disorders. For example, blurry and glary vision can occur with cataracts, but can also occur with glasses problems. Therefore, the only way to definitively detect the presence of early cataract development is with a slit lamp exam (see diagnostic services for more detail) through a dilated pupil. This is usually done as part of a comprehensive eye examination.
Many of the symptoms of cataract development can occur with other ocular disorders. For example, blurry and glary vision can occur with cataracts, but can also occur with glasses problems. Therefore, the only way to definitively detect the presence of early cataract development is with a slit lamp exam (see diagnostic services for more detail) through a dilated pupil. This is usually done as part of a comprehensive eye examination.Do cataracts affect both eyes?
Is a cataract the same as macular degeneration or glaucoma?
Can cataracts be prevented?
In most cases, there is no way to prevent the development of cataracts. There are however several things that one can do to perhaps slow down the progression of cataracts:
- Wear protective eyewear when necessary.
- Avoid prolonged exposure to ultraviolet light. Wear UV protective eyewear when outdoors in bright sunlight long enough to get a sunburn.
- Maintain a healthy lifestyle. While there is no universal agreement on the effects of smoking and cataract development, many believe that there is a relationship. Eating foods rich in anti-oxidants may be helpful. There are studies that show that high doses of Vitamin C slows the progression of age-related cataract development. Other studies are being done investigating other anti-oxidants and their effect upon cataract development.
- Maintain control of your diabetes. Elevated blood glucoses over a long period of time can accelerate the progression of cataracts.
Can cataracts be treated besides having surgery?
If I have to have cataract surgery, what can I expect during the operation and afterwards?
What does “no-stitch, no needle” cataract surgery mean?
What are the current methods of cataract surgery? Is there such a thing as “laser” removal of cataracts?
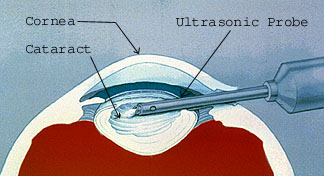
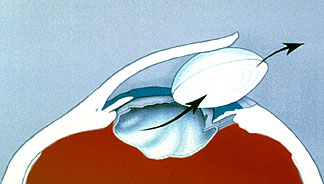

There are generally three methods of cataract surgery that can be used: PHACOEMULSIFICATION: This technic is a highly advanced method of cataract removal and has been the favored technic at Davidson Eye Associates for over 25 years. Here, an ultrasonic oscillating probe is inserted into the eye through a tiny incision no larger than a puncture wound. The probe breaks up the center of the cataract into extremely tiny pieces. The fragments are then suctioned from the eye at the same time. After the cataract is removed, a lens implant (see question 15 for details on lens implants) is permanently inserted into the eye to help focus light rays onto the surface of the retina as the natural lens used to do before it turned into a cataract. The incision created is so small that it rarely requires any stitches to close, and usually requires no more than numbing drops to do the procedure. The advantages of this technic is that the eye heals rapidly allowing patients to resume normal activities almost immediately in most cases. It is considered by many as a safer operation because of a small wound size, and it causes little astigmatism changes in the eye. EXTRACAPSULAR CATARACT EXTRACTION (ECCE): Still used in some cases, this technic involves removing the center of the cataract all in one piece using a rather large incision into the eye. More anesthesia is usually required in the form of IV sedation, and injections of numbing medicine around the eye is necessary for maximum safety. The numbing injections are usually not felt by the patient because of the sedation. Because of a larger incision, stitches are required. Such stitches are finer than human hair and are generally not felt by the patient. There are generally more limitations following ECCE, and discomfort is usually minor as with phaco-emulsification. Patients generally experience excellent visual results as well when this technic is used. For many surgeons that practice phaco-emulsification as their primary method of cataract removal, ECCE is still occasionally necessary for unusually hard or large cataracts and may be a safer operation for such cataracts. LACS (Laser Assisted Cataract Surgery): There has traditionally been much public confusion and misinformation over the term “laser” as it applies to cataract surgery since many surgery advertisements in the past inaccurately use the word “laser” to describe “phacoemulsification.” However there is now technology that allows part of the cataract surgery do be done using laser technology. There is currently debate on the advantages/disadvantages of this new and upcoming technology. LACS does not replace phacoemulsification but is used in some steps of the cataract procedure. Either way, this technology will continue to advance, but still has a ways to go. Patients should understand however that even with future laser technology, an incision into the eye will always be necessary.
What exactly is a lens implant? Is it the same thing as an eye transplant?
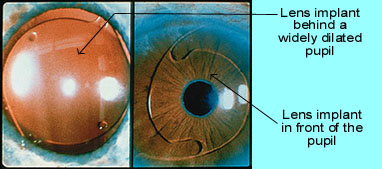
 During cataract surgery, the natural lens of the eye that “turned bad” is removed resulting in a loss of focusing power for the eye. This situation would be similar to taking photographs without a camera lens. The pictures would be extremely blurred. When the natural lens of the eye is removed, a lens of some sort must be used for the eye to focus.Years ago, when patients had cataract surgery, they wore thick cataract glasses to do the focusing that their natural lens did before it turned into a cataract. Later on, special contact lenses were developed to allow cataract patients to focus. Many older adults however had trouble managing them, and infection was a problem for patients who slept in them. Soft foldable IOL For the past 40 or so years, intraocular lenses (IOL’s or “lens implants”) have evolved with amazing success, and lens implantation is now considered a standard part of cataract surgery. The IOL is a tiny, lightweight, clear plastic lens placed in the eye, usually in the same location as your natural lens, which replaces the natural lens of the eye that turned into a cataract. The IOL remains a permanent part of the eye for a lifetime and only in extremely rare circumstances becomes troublesome. IOL’s can be a hard plastic, soft plastic, or soft silicone. At Davidson Eye Associates, we use predominantly a soft acrylic that actually folds, allowing placement into the eye through the same tiny puncture-like insicion used for cataract removal. The lens is placed in proper position and allowed to unfold in the eye. Such technology shortens the recovery time following surgery. IOL designs, materials, and implantation technics continue to evolve.
During cataract surgery, the natural lens of the eye that “turned bad” is removed resulting in a loss of focusing power for the eye. This situation would be similar to taking photographs without a camera lens. The pictures would be extremely blurred. When the natural lens of the eye is removed, a lens of some sort must be used for the eye to focus.Years ago, when patients had cataract surgery, they wore thick cataract glasses to do the focusing that their natural lens did before it turned into a cataract. Later on, special contact lenses were developed to allow cataract patients to focus. Many older adults however had trouble managing them, and infection was a problem for patients who slept in them. Soft foldable IOL For the past 40 or so years, intraocular lenses (IOL’s or “lens implants”) have evolved with amazing success, and lens implantation is now considered a standard part of cataract surgery. The IOL is a tiny, lightweight, clear plastic lens placed in the eye, usually in the same location as your natural lens, which replaces the natural lens of the eye that turned into a cataract. The IOL remains a permanent part of the eye for a lifetime and only in extremely rare circumstances becomes troublesome. IOL’s can be a hard plastic, soft plastic, or soft silicone. At Davidson Eye Associates, we use predominantly a soft acrylic that actually folds, allowing placement into the eye through the same tiny puncture-like insicion used for cataract removal. The lens is placed in proper position and allowed to unfold in the eye. Such technology shortens the recovery time following surgery. IOL designs, materials, and implantation technics continue to evolve. 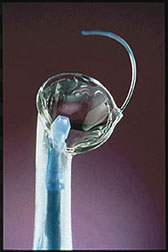 An IOL or “lens implant” is different that an “eye transplant,” which is a term that actually means a “corneal transplant.” The cornea is the front part of the eye (see Anatomy of the Eye for details) that functions like the window for your vision. Like the lens, the cornea has enormous focusing power for the eye. Some diseases can cause permanent clouding of the cornea making it necessary to replace the cornea in order to see again. These corneas come from patients who have donated their eyes at their death. The corneas are preserved in an eye bank.
An IOL or “lens implant” is different that an “eye transplant,” which is a term that actually means a “corneal transplant.” The cornea is the front part of the eye (see Anatomy of the Eye for details) that functions like the window for your vision. Like the lens, the cornea has enormous focusing power for the eye. Some diseases can cause permanent clouding of the cornea making it necessary to replace the cornea in order to see again. These corneas come from patients who have donated their eyes at their death. The corneas are preserved in an eye bank.
 Blind eye due to corneal scarring Blind eye due to corneal scarring |
 Removal of scarred cornea in preparation for a donor cornea Removal of scarred cornea in preparation for a donor cornea |
