- How does diabetes cause blood vessel disease?
- What is diabetes mellitus?
- What is diabetic retinopathy?
- How does blindness occur with diabetic retinopathy?
- Who gets diabetic retinopathy?
- Can diabetic retinopathy be prevented?
- What about laser treatment for diabetic eye disease?
How does diabetes cause blood vessel disease?
Insulin allows blood sugar to enter the cell where is it burned for fuel. All cells in the body need glucose, and insulin functions as the key to let glucose in. Without proper utilization of insulin, blood glucose become high, and the body “deals” with this high level of glucose in different ways. Much of it is eliminated by the kidneys, and some is handled by the liver where it is converted into other compounds such as fat and protein. Glucose also is converted into other types of sugars for storage such as sorbitol and fructose, both of which can be damaging to blood vessels. Generally, blood vessel walls become thickened, and capillaries start to close leading to reduction in tissue circulation. Blood vessel support structures decrease leading to microaneurysms. As blood vessel walls deteriorate, they begin to leak blood components into the retinal tissue. This along with reduction in circulation sets up a cascade of events that left untreated, lead to retinal swelling, hemorrhage, scar formation within the cavity of the eye, and subsequent retinal detachment.
What is diabetes mellitus?
Diabetes Mellitus is a disorder in which glucose, commonly known as “blood sugar” is not properly utilized by the body resulting in abnormally elevated levels. There are many hormones that the body uses to regulate blood sugar so that they remain in normal range. Hormones that elevate blood sugar include growth hormone, glucocorticoids, epinephrine, and others. However insulin is the only hormone in the body that lowers it making insulin an extremely precious commodity. Type I diabetes, previously called juvenile-onset or insulin-dependent diabetes, occurs when the beta islet cells of the pancreas are destroyed leading to an absolute insulin deficiency. Here, insulin needs to be given on a daily basis. Type II diabetes, previously called adult-onset or noninsulin-dependent diabetes, is a combined mechanism of low levels of insulin secretion and the body’s inability to use it.
90% of all patients with diabetes have the Type II form, and 10% the Type I form. Diabetes is considered a “vascular” disease, and major organ complications involve the heart, kidney, and eye. There is general agreement that the severity of elevated blood glucoses (hyperglycemia) and duration of the disease are the major risk factors for developing long term complications. Many physicians also believe that other factors are important such as age, type of diabetes, weight, smoking, and other medical problems such as hypertension although there is less agreement among many studies.
What is diabetic retinopathy?
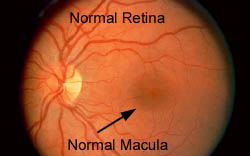
The part of the eye most commonly affected by diabetes is the retina. Because of blood vessel
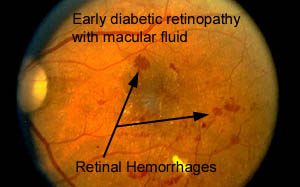
damage, the retinal circulation becomes compromised leading to a cascade of events that destroy the retina and vision. The earliest stage of diabetic retinopathy is the “non-proliferative” stage, with the formation of microaneurysms and tiny hemorrhages in the retinal tissue. At this level, there is usually no noticeable visual change. Patients may be unaware that there is anything wrong with their eyes. Increasing blood vessel leakage however leads to swelling of the retina. When the swelling begins to involve the macula,vision problems often become very noticeable. (For more information about the macula, please click on The Anatomy of The Eye and How It Works, and Macular Degeneration.)
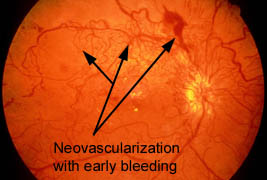
As the disease progresses, blood vessels begin to close off leading to poor circulation of the retina. This results in increasing hemorrhages, fluid leakage, and the formation of new but very dangerous blood vessels.
This process of laying down new blood vessels is called neovascularization, and is in a sense the retina’s attempt to better oxygenate itself. This advanced stage of retinopathy is called “proliferative”
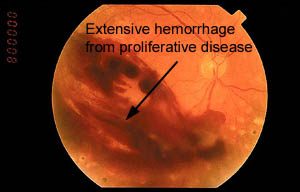
retinopathy. These new blood vessels are prone to bleed, resulting in intraocular hemorrhage, the laying down of scar tissue, glaucoma, and retinal detachment.
How does blindness occur with diabetic retinopathy?
The mechanism for visual loss with DR is complex:
- Macular Edema: Basically this is when fluid from leaky blood vessels accumulate in the macular area of the retina. The macula serves your central vision and does not tolerate the presence of fluid well. Fluid causes degredation of macular function, and with time, does irreversible damage to the macula.
- Macular Ischemia: Ischemia is a medical term meaning poor circulation to tissue. In macular ischemia, macular function is poor because of poor oxygenation. There is irreversible decline in central vision over time.
- Proliferative Diabetic Retinopathy (PDR): An advanced form of retinopathy where friable new vessels grow in and on the surface of the retina. They are prone to bleed, resulting in hemorrhaging in the eye. They also form scar tissue in the eye which can lead to retinal tears and detachment. Glaucoma can also occur in advanced PDR.
Who gets diabetic retinopathy?
Diabetic retinopathy is the leading cause of new cases of legal blindness among working-age Americans. Sixteen million Americans have diabetes. Duration of the disease along with elevated blood sugars are the major risk factors with this blinding illness. It is estimated that 25% of type 1 diabetics will have some form of retinopathy after 5 years, and 80% will have retinopathy after 15 years.
In type 2 diabetics who are on insulin, 40% will have some form of retinopathy after 5 years. For those who take diabetic medication by mouth, 24% will have retinopathy after 5 years. This jumps up to 83% and 53% respectively at 19 years duration.
Can diabetic retinopathy be prevented?
Although diabetes itself currently cannot be prevented, its complications including diabetic retinopathy can be delayed or moderated. The Diabetes Control and Complications Trial (DCCT) showed that lowering blood sugar and maintaining glucose levels at near normal reduced vital organ complications including the eye. Another study called the United Kingdom Prospective Diabetes Study (UKPDS) confirmed this and also emphasized the need to control blood pressure in diabetics who were hypertensive. The prevention and early detection process is as follows:
- Maintaining blood sugar and hemoglobin A1c levels as near normal as is safely possible.
- Control of other medical problems such as hypertension and fat levels such as cholesterol
and triglycerides. - Comprehensive Examination by an ophthalmologist experienced in managing diabetic retinopathy. Generally, patients under 30 years of age should have a comprehensive eye exam within 5 years of diagnosis of diabetes. Thereafter, eye exams should be yearly. Over the age of 30 years of age, patients should have an eye exam at the time of diagnosis, and yearly thereafter. If retinopathy if found, the frequency of examinations will vary according to the
degree of retinal involvement. As part of a comprehensive exam, other diagnostic tests such as gonioscopy, visual fields, fundus photography, and fluorescein angiography may be needed if retinopathy is found. (For a description of these tests, please click onto diagnostic services.) - Other health measures with varying levels of agreement include maintaining weight control,
exercising, eating a well balanced diet, and avoidance of smoking.
What about laser treatment for diabetic eye disease?
Fortunately the armamentarium for combating diabetic retinopathy is growing with more awareness, better capabilities for detecting early disease, the growing emphasis for better blood sugar control, and better ways of treating diabetic eye disease. Observation is often possible in patients with diabetic retinopathy who may continue to enjoy good vision for years. However medical management of diabetes during early retinopathy is extremely important and should include: keeping down blood sugars as much as safely possible, eating a well balanced diet, cessation of smoking, losing weight, controlling other medical problems such as hypertension, elevated lipids, etc.
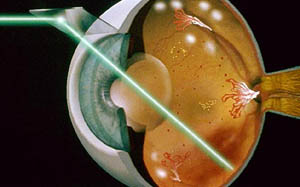 If diabetic retinopathy progresses to where vision is threatened, laser treatment or surgery are often helpful in preventing blindness. Treatment can be complicated and may involve not only your ophthalmologist, but also other medical doctors and retinal specialists. Laser treatment is often reserved for macular edema (swelling of the macular area) and proliferative disease where new blood vessels are being formed that threaten the retina. The goal of laser treatment for macular swelling is to limit or prevent further damage to central vision, not necessarily improvement of vision. The risk of visual loss is reduced by 50% for those who undergo appropriate laser treatment as compared to those who are not treated.
If diabetic retinopathy progresses to where vision is threatened, laser treatment or surgery are often helpful in preventing blindness. Treatment can be complicated and may involve not only your ophthalmologist, but also other medical doctors and retinal specialists. Laser treatment is often reserved for macular edema (swelling of the macular area) and proliferative disease where new blood vessels are being formed that threaten the retina. The goal of laser treatment for macular swelling is to limit or prevent further damage to central vision, not necessarily improvement of vision. The risk of visual loss is reduced by 50% for those who undergo appropriate laser treatment as compared to those who are not treated.
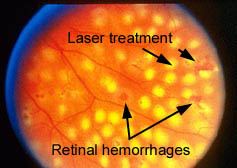 Laser treatment for proliferative disease is more extensive than for macular edema. The goal is to limit or end the growing of new blood vessels which can bleed and eventually cause scarring and retinal detachment. In all cases of laser treatment, the goal is stabilization of vision and preventing further damage and blindness. Risks of laser treatment include loss of vision, worsening of vision, washed out colors, decreased night vision, and loss of peripheral vision. In most cases of retinopathy requiring laser treatment, the benefits of treatment far outweigh the consequences that occur without treatment.
Laser treatment for proliferative disease is more extensive than for macular edema. The goal is to limit or end the growing of new blood vessels which can bleed and eventually cause scarring and retinal detachment. In all cases of laser treatment, the goal is stabilization of vision and preventing further damage and blindness. Risks of laser treatment include loss of vision, worsening of vision, washed out colors, decreased night vision, and loss of peripheral vision. In most cases of retinopathy requiring laser treatment, the benefits of treatment far outweigh the consequences that occur without treatment.