- What is age related macular degeneration (AMD)?
- Are There Different Types of Macular Degeneration?
- How Is AMD Detected?
- Does AMD Cause Total Blindness?
- Can the Dry Form of AMD Lead to The Wet Form?
- Can AMD in One Eye Progress to the Other?
- What Is a Macular Hole? Is This the Same Thing as AMD?
- What Is Macular Pucker? Is This Another Name For Macular Degeneration?
- Is AMD Hereditary?
- Can Sunlight Exposure Affect AMD?
- What Are the Risk Factors for Developing AMD?
- What Role Does Nutrition Play in Controlling, Helping, or Preventing AMD?
- What treatment is currently available for AMD?
- Is this new PDT laser treatment a cure for AMD?
- Is there a video I can watch that explains what Macular Degeneration is?
-
What is age related macular degeneration (AMD)?
Age related macular degeneration (AMD) is a leading cause of poor vision after age 60 currently affecting approximately 10 million Americans and millions more around the world. This disease attacks the macula, that part of the retina where your central “eagle eye” vision occurs. Although macular degeneration rarely causes “complete” blindness, it often destroys central vision leaving only the peripheral (“outermost”) vision intact. To learn where the macula is in relation to other parts of the eye, click eye anatomy for an overview of how the eye works.
-
Are There Different Types of Macular Degeneration?
There are many types of macular degeneration and many causes. The fastest growing form is AMD or Age-Related Macular Degeneration and accounts for 90% of new cases of legal blindness in the US. In this category, there are basically 2 types: dry and wet macular degeneration. The “dry” form is usually a slow form of macular deterioration which may take years before loss of central vision occurs. Nine out of 10 people with AMD will have the dry form. Also, many times, visual loss will “plateau” with long periods of visual stability occurring. Visual loss can range from mild to severe.
The “wet” form accounts for approximately 10% of cases of AMD and is much more severe. It is called “wet” because abnormal blood vessels invade the macular area causing leakage of fluid and blood, which can then accumulate under the macular area and cause damage to cellular elements. The damage is permenant and cannot be repaired. Sometimes, laser treatment can be helpful in limiting the amount of damage to the macula. (See below) Below is a photo of advanced “wet” AMD.
- This is a photo of advanced “wet” AMD.
- Normal picture of the retina. The dark spot in the center of the picture is the macula, and is approximately 1/16th inch in diameter. The yellow spot to the left is the optic nerve.
Non-age causes of macular degeneration can include nutritional deficiencies, sun gazing, ocular injuries, head injuries, certain medication reactions, and certain other systemic diseases such as diabetes and chronic uncontrolled hypertension. High refractive errors such as myopia (nearsightedness) is also associated with macular degeneration.
-
How Is AMD Detected?
 Visual blur, loss of detailed vision, distortion, are some of the possible symptoms of AMD. However it is important to understand that many disorders of the visual system can present with similar symptoms. For example, a change in glasses prescription or the development of cataract disease both can cause visual blur. Sometimes, AMD can be totally without visual symptoms. The only definitive way to diagnose AMD is with a retinal examination by a trained professional such as an ophthalmologist.
Visual blur, loss of detailed vision, distortion, are some of the possible symptoms of AMD. However it is important to understand that many disorders of the visual system can present with similar symptoms. For example, a change in glasses prescription or the development of cataract disease both can cause visual blur. Sometimes, AMD can be totally without visual symptoms. The only definitive way to diagnose AMD is with a retinal examination by a trained professional such as an ophthalmologist.
-
Does AMD Cause Total Blindness?
AMD does not cause TOTAL blindness, but only loss of central vision. Your peripheral vision generally will remain intact except for highly advanced cases of wet AMD. Other disorders, however, can cause problems with your peripheral vision such as cataracts and glaucoma.
-
Can the Dry Form of AMD Lead to The Wet Form?
An amsler grid is a chart of uniform squares. In the center of the chart is a black spot. In testing your vision, cover one eye, and fixate your vision on the center spot. At the same time, observe the squares in your side vision. They should look even. Any distortion is cause for concern as seen in this example.
Most cases of dry AMD remain that way, although there are forms of dry AMD that are at high risk of developing into the wet type with time. If your ophthalmologist feels that you are at risk for developing the wet form, he will generally have you do self-testing at home with a special chart called an Amsler Grid.
-
Can AMD in One Eye Progress to the Other?
AMD affects both eyes in the vast majority of cases, although it is common for one eye to be more affected than the other. If only one eye is involved, you are very likely to develop some involvement in the other in time. Many cases of “dry” macular degeneration remain stable for years, and others can progress slowly. Still other cases can develop “wet” macular degeneration where rapid deterioration of central vision often occurs.
-
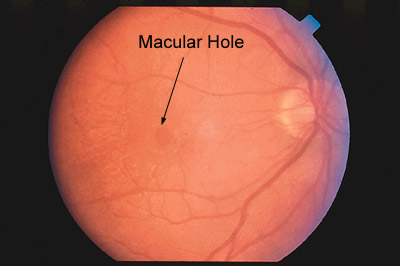
What Is a Macular Hole? Is This the Same Thing as AMD?
Macular holes and macular degeneration are 2 different conditions. Because both affect the macula, the symptoms may be the same. Macular holes usually begin with mildly blurred or distorted vision, and over time can result in loss of central vision. The peripheral vision is not affected. Macular holes have a higher rate of occurrence in women for reasons we do not fully understand, and 90% of the time involve only one eye. Unlike macular degeneration, there are no dietary recommendations for macular holes. There is a surgical procedure available to close the macular hole with varying degrees of success for visual improvement.
-
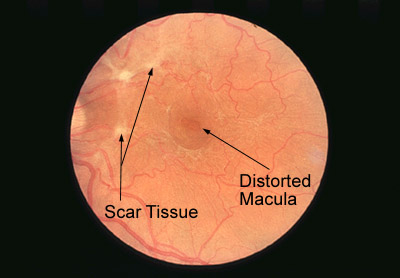
What Is Macular Pucker? Is This Another Name For Macular Degeneration?
Macular pucker is not the same thing as macular degeneration although it does affect the macula. In macular pucker, a thin layer of scar cells grows across the macula. With time, this thin layer of scar contracts causing wrinkling of the macular surface. This results in distorted vision. The majority of the time, macular pucker is well tolerated visually with only mild amounts of visual decrease. For moderate amounts of central visual loss or distortion, surgery to remove the surface scar tissue can be done. Severe complications to this surgery are rare and can be helpful, although the vision rarely returns to normal.
-
Is AMD Hereditary?
There are many factors involved in the development of AMD, but there is clearly a genetic component. Your risk of AMD is higher if there are other family members who have it. We don’t fully understand how the genetics work or what particular genes are “responsible” for AMD. Much research is concentrated on the genetic aspect of this disease, and if a gene is involved, why some family members contract it, and other don’t. There are other factors that appear to increase the risk and which seem to contribute to AMD (Risk factors are addressed elsewhere in this FAQ).
-
Can Sunlight Exposure Affect AMD?
Except for deliberate sungazing which can permanently damage the macula, the role of casual unprotected sun exposure causing or worsening AMD is controversial. Studies have reached conflicting results. At present, there is no conclusive proof that long-term sun exposure increases the chance of developing AMD. However, it is believe that sun exposure tends to increase the chance of developing cataracts. Many ophthalmologists will advise older adults to wear a sun visor of UV protected sunglasses if out in the sun long enough to cause a mild sunburn.
-
What Are the Risk Factors for Developing AMD?
It is helpful to think in terms of risk factors that YOU CAN CONTROL, and those that YOU CANNOT CONTROL.
“Controllable” Risk Factors:
- Smoking: There appears to be a corrolation between smoking and AMD. The exact
mechanism is not clear, but many believe that it has to do with the generation of “free radicles” (harmful by-products of normal body metabolism) and their damage to body tissues. Also, tobacco appears to interfere with the absorption of lutein, and important antioxidant that protects the retina from damaging free radicles.
- Hypertension: The link between high blood pressure and AMD is well established. Remember, there are often no symptoms of high blood pressure. A regular check up is the best way to have a clear handle on any medical problems that you may have.
- Exposure to ultraviolet sunlight: Still controversial. (See question 10)
- Proper nutrition: What role nutrition or nutritional substances have on AMD is still very controversial. There is a growing body of knowledge however that suggests that deficiencies in diet and certain nutritional substances could play a role in AMD. There continues to be a raging debate too on the role of antioxidants in AMD. Generally, the diet widely recommended as beneficial for cardiovascular good health – low in fat, high in dark green leafy vegetables and fruits – may be helpful in patients with AMD.(See question 12)
“Uncontrollable” Risk Factors:
- Age: Risk for AMD increases with increasing age.
- Race: AMD is more common in Caucasians than other races.
- Eye color: AMD is more common in blue eyed people, due to perhaps less protective pigment in their eyes.
- Severe farsightedness (hyperopia) or nearsightedness (myopia)
- Genetics (See question 9)
- Smoking: There appears to be a corrolation between smoking and AMD. The exact
-
What Role Does Nutrition Play in Controlling, Helping, or Preventing AMD?
This is a topic that is currently highly controversial, and there are no studies that are conclusive that dietary supplementation affects the long term outcome of AMD or does anything to prevent it. Designing scientific studies is difficult due to the fact that AMD, particularly the dry form, progresses slowly over a long period of time. When AMD is discovered in a patient, often their dietary history over the past 20 – 30 years remains illusive. Also the definitions of what constitutes a good diet has changed. However, the body of knowledge regarding the role of vitamins, minerals, and herbals is exploding, and
will redefine the issues of wellness and disease prevention in the not-to-distant future.There is a growing body of evidence that antioxidant vitamins and minerals incorporated into supplemental products may be effective slowing down or reversing eye disease. Although mostly published in nutritional journals, more are being published in medical journals. Regarding AMD, there has been a great deal of attention among researchers regarding nutritional supplements and reduced incidence and severity of macular degeneration. There is a very practical debate, however, for supplemental nutrition. Some points of issue include the following:
- A growing concern over food processing and environmental stresses upon health and maintaining health.
- Lack of time or inclination to eat properly, especially among older adults living alone.
- Demineralization of our soil that is sorely lacking in selenium, and is low on zinc, magnesium, calcium, and others.
- Report by the American Medical Association (AMA) showed that nearly 90% of Americans do not get even the RDA of essential vitamins and minerals.
- Despite the recommendations of the National Cancer Institute to consume 5 servings of fruits and vegetables per day, less than 10% of Americans eat 2 – 3 servings of fruits and vegetables, and at least 50% of Americans eat no vegetables,
and 70% eat no fruits or vegatables rich in vitamin C (from The Real
Vitamin and Mineral Book, Lieberman et al.). - While little can be done to alter genetic predisposition to disease, much can be done environmentally, particularly nutrition and water supply that can greatly help.
- The “modern” diet features an increased intake of fats and sugars, and less with complex carbohydrates and fibers and an inadequate intake of essential vitamins and minerals. Many experts feel that it is impossible to meet the RDIs by eating the
food available today. - Many people currently are seeking ways to attain a longer and healthier life. The public is becoming more savvy in health issues and is looking for leadership in wellness.
- Certain terms must be understood to make the following discussion regarding nutrition and AMD meaningful to you.
DEFINITIONS
VITAMIN
Natural occuring organic compounds in plants and animals that work with other enzymes to allow chemical reactions to occur in your body. Fat Soluble Vitamins: A,D,E,K, and Water Soluble Vitamins B complex and C.MINERAL
Elements not produced by plant or animal. Like vitamins, they function as coenzymes that allow chemical reactions to occur in your body. There are the macro or “bulk” minerals such as calcium, and micro or “nutrient” minerals such as zinc and copper.HERB
Any plant whose stems and leaves wither after the growing season each year. Can be used as a medicine, seasoning, etc.FREE RADICAL
Unstable oxygen atoms and other compounds produced in every cell of the body that generate oxidative damage to cells and tissues causing degenerative disease.ANTIOXIDANT
Compounds that neutralize free radicals.BIOFLAVONOID
Compounds found in plants that normally give vegetables and fruit their normal color. They function as a helper to the body’s immune system, and they act as scavengers of free radicals.ENZYME
Catalysts or activators of chemical reactions that continuously take place in your body. Enzymes make things happen and happen faster. They are necessary for all body functions.ORGANIC
Having to do with or come from life. Carbon is the backbone of all organic compounds.INORGANIC
Not having been produced by plant or animal.RDA
“Recommended Daily Allowance”. Minimum daily requirement of micronutrients to prevent deficiency diseases. Based upon gender, age, etc. Cumbersome. Inadequate to promote wellness.RDI
“Reference Daily Intake”. Replaced RDA in 1997 as the official term and represents average need for persons older than four years of age. Based upon 2,000 cal for women and 3,000 cal for men.ODI
“Optimum Daily Intake”. Nutrient requirement to attain a state of optimum health according to Lieberman and Bruning.Understanding “free radicles” is important and perhaps central to understanding the current thinking about supplementation for AMD. Free radicles are by-products produced
by every living cell in the normal course of metabolism, and are atoms or groups of atoms with one or more unpaired electrons. This results in electrochemical instability in which free radicles then interact with other cells taking or giving electrons randomly. This in turn destabilizes molecules in cell walls and other cellular structures causing a cascade of events that lead to cellular destruction. This is thought to be one of the factors in the normal aging process of the body. Free radicles, however, do some good to the body as well such as fighting off infection.What are antioxidants, and what role do they play in AMD?
In thinking about free radicles in the course of degenerative disease such as AMD, antioxidants are substances that neutralize and significantly inhibit the rate at which free radicles operate, keeping down the population of these destructive elements. There are vitamin antioxidants such as vitamins A, E, and C; mineral antioxidants such as
zinc and selenium; and bioflavenoid antioxidants such as grape seed, citrus extract, and carotenoid pigments such as the carotenes and xanthophylls.It is believed by many that free radicles play some role in AMD although the exact mechanism is not clear. The substances that you may hear most about regarding AMD are zinc, lutein and zeaxanthin.
Lutein is a xanthophyll and is found in spinach, kale, collard and mustard greens, and egg yolks. Lutein is the only xanthophyll that accumulates in the eye, specifically the macula. Closely related to lutein is zeaxanthin which seems to produce a thicker, more protective macular pigment. It is thought that a diet rich in these compounds increases the density of macular pigments.
Zinc is a common trace mineral and is highly concentrated in the eye, particularly in the retina and macular areas. Some studies have shown that zince levels are low in some
older adults either because of poor diet or poor absorption of zinc from food. Because zinc is so important for the health of the macula, come doctors think that zinc supplementation may slow the process of AMD. Scientific studies here are also imcomplete, however, and there is no agreement among doctors concerning the value of zinc supplementation. Too much zinc also can interfere with other important trace minerals such as copper.Should you consider nutritional supplementation?
As it relates to AMD, it might be prudent if: 1) you are over the age of 50, 2) have a family history of AMD, 3) have AMD yourself, 4) have insufficient dietary intake of vitamins
and minerals. Keep the following points in mind, however.- Researchers do not agree if nutritional supplementation is helpful in AMD, although it is well recognized that for many, nutrition is not optimal, and that carefully formulated supplements may be helpful.
- Supplements should not be an easy way out from a balanced diet with foods rich in vitamins and minerals.
- Do not supplement yourself without medical guidance from your physician. With supplements being available at every corner and through many catalogues, many fall prey to the lastest fads. Remember that too much of a good thing can be harmful, especially with fat soluble vitamins and certain herbs, and high doses of trace minerals. For example, the New England Journal of Medicine (1996) reported an increased risk of acquiring lung cancer with 25,000 units of vitamin A and 30 mg
of beta-carotene taken on a daily basis. - Remember that while nutritional issues may contribute to the onset or worsening of AMD, other factors too have been implicated. (See question 11)
-
What treatment is currently available for AMD?
Please review questions 11 and 12. For the dry form, minimizing the risks, maintaining optimal health and diet, controlling other medical problems such as hypertension and diabetes, remain the cornerstone of treatment. Observation of your AMD is also necessary and may need to be evaluated as often as every couple of months to yearly. Also your ophthalmologist may have you do self testing with an amsler grid while at home and between office visits.
The wet form of AMD may be treatable with laser and can prevent further visual loss if caught in time, depending upon a variety of circumstances such as its location relative to the macula, the size of the area involved, and other factors. Conventional laser treatment however is limited in that it generally is not used if the center of the macula is involved. This is because the laser will destroy macular tissue at the same time it destroys the abnormal blood vessels. It is used however when blood vessel growth occurs outside the center of the macula and threatens damage. Some ophthalmologists will use the laser in the center of the macula when central vision is lost in order to limit the size of the resultant blind spot that occurs in the center of the vision in this disease.
(Please see queation 14 for discussion of new laser treatment for wet AMD.) -
Is this new PDT laser treatment a cure for AMD?
PDT or photodynamic therapy is a type of laser therapy for certain types of wet AMD and is considered a break through for patients with wet AMD that otherwise could not be treated with conventional laser therapy. It is estimated that 200,000 new cases of the “wet” form of AMD are diagnosed each year. Unfortunately, the options for treating wet AMD are limited. PDT is considered a “breakthrough” and offers hope to such cases that would have been determined as untreatable. How does it work? Read on.
The difference between conventional laser treatment for wet AMD and PDT is that conventional laser treatment destroys retinal tissue as it destroys the abnormal blood vessels that threaten macular destruction. Therefore treatment of abnormal blood vessel growth within the macular area is impossible because the macular area itself would be destroyed. In PDT, a “light-activating” dye called verteporfin or Visudyne™ is injected intravenously and is absorbed by the abnormal blood vessels. A special nonthermal laser is then applied to the macular area and activates the drug. This chemically changes the drug into a complex that stops leakage without damaging normal retinal or macular tissue.
While the possibilities have expanded treatment options, there are some drawbacks currently. Most patients will need to be re-treated at 3-month intervals during the first year. 2 year studies are not out yet. Of course, with each treatment, a fluorescein angiogram will be needed. Patients on verteporfin treatment will need to avoid bright light or sunlight due to the skin damage that can occur with light exposure until the dye is completely out of the body system. This includes exposure to halogen lighting, tanning salons, and the kind of lighting used in operating rooms or dental offices. Sunglasses and long sleeve clothing are necessary. Also, not all cases of wet AMD are candidates for PDT treatment as it exists now. The treatment decision can be complicated and can only be determined by your ophthalmologist. It is expected however that we are only at the tip of the iceberg, and treatment possibilities and guidelines are expected to change dramatically in the next several years.
-
Is there a video I can watch that explains what Macular Degeneration is?
Certainly! Just click on the video below for further information. Also click here for our video educational journal page about other ocular disorders and treatments!.


