- What is glaucoma, and how prevalent is the disease?
- What causes glaucoma?
- Are there different kinds of glaucoma?
- Who gets glaucoma?
- Are there risk factors for the development of glaucoma?
- What’s the difference between a glaucoma suspect and a glaucoma patient?
- How can I tell if I have glaucoma?
- Is glaucoma painful?
- How is glaucoma diagnosed?
- What is the treatment for glaucoma?
- How does laser treatment work for glaucoma? Is the treatment painful?
- When is surgery necessary for treatment of glaucoma?
- How often should I have my eyes examined for glaucoma?
- Is there a video I can watch that explains Glaucoma?
-
What is glaucoma, and how prevalent is the disease?
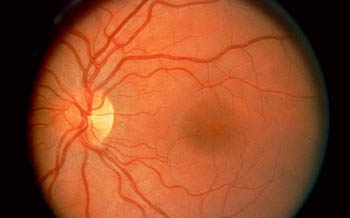
Normal picture of the retina. The dark spot in the center of the picture is the macula, and is approximately 1/16th inch in diameter. The yellow spot to the left is the optic nerve.
Approximately 1.2 million nerve fibers from the retina come together and form a “cable” called the optic nerve. This nerve connects the back of the eye to the brain. When light bounces off an image and strikes the retina, it organizes and “packages” the image, and sends the electrical impulses to the brain via the optic nerve. The brain then “decodes” these electrical stimuli into what we know as vision.
Glaucoma is a disease that causes damage to the optic nerve which threatens blindness. The optic nerve is the “cable” that connects the eye with the brain and which carries visual information from the retina (back of the eye) to the seeing centers of the brain. (See Eye Anatomy for details.) The optic nerve is composed of over one million nerve fibers and is approximately 1/16th of an inch in diameter. There are many forms and causes of glaucoma (see below) which can be extremely difficult disease to diagnose at times.
Glaucoma is considered a major health problem, and it is estimated that over 2 million Americans have the disease, and as much as half of them may be unaware of the problem. Every year, as much as 100,000 Americans develop glaucoma. According to the American Academy of Ophthalmology, in the United States alone, glaucoma of all types is the second most common cause of legal blindness, and is the leading cause of legal blindness among African Americans. Approximately 80,000 Americans are legally blind from glaucoma, and many more have visual impairment. Glaucoma is one of the most common causes of preventable blindness. There is no cure for glaucoma. However, with proper treatment, blindness can be prevented in 90% of the cases.
-
What causes glaucoma?
The eye is a closed cavity that has its own internal fluid circulation which bathes and nourishes the internal eye. This fluid is called aqueous humor and is made by tiny glands in the ciliary body, a muscle that helps the eye focus. This muscle is located behind the iris (the colored part of the eye).
Internal Circulation of the Eye (Red Arrows): Aqueous (watery fluid) is made from the glands located in the ciliary body. It then circulates in the posterior chamber where it bathes the iris and lens. It flows through the pupil and into the anterior chamber where it nourishes the cornea, and finally empties back into the blood stream after passing through the trabecular meshwork and into Schemm’s Canal.Aqueous (red arrows) then flows from behind the iris, through the pupil, and into the front compartment of the eye (called the anterior chamber) where is nourishes the cornea and lens. From there, it is normally drained out of the eye through a filtering drain called the trabecular meshwork. The trabecular meshwork is situated in the angle of the eye (where the colored and white parts of the eye meet. In many cases of glaucoma, this “drain” becomes clogged such that fluid cannot leave the eye as fast as it is produced. This causes fluid pressure to build up in the eye. Optic nerve damage in glaucoma is usually caused by this elevated fluid pressure within the cavity of the eye.
Although most cases of glaucoma are related to abnormally elevated fluid pressure in the eye, the degree of fluid pressure elevation necessary to cause optic nerve damage varies
from individual to individual. Many people tolerate elevated pressures without any optic
nerve damage at all. Still others can have severe optic nerve damage with normal or only mild elevations of pressure. In these types of patients, it is thought that optic nerve damage is a result of poor blood flow to the nerve making the nerve very sensitive to pressure in the high normal range. -
Are there different kinds of glaucoma?
-
Who gets glaucoma?
It is not an understatement to say that EVERYONE, children to older adults, should be concerned about glaucoma, because early detection and treatment are the only ways to prevent irreversible blindness. See below for risk factors that place certain people at greater risk.
-
Are there risk factors for the development of glaucoma?
There are several conditions that put some people at greater risk:
-
- Age. Although glaucoma can occur in younger persons, the risk for glaucoma increases with age, generally beyond 40.
- Family History. Glaucoma can be inherited, and therefore family history is a risk factor. The Baltimore Eye Survey found that open-angle glaucoma is increased approximately 3.7 fold for individuals having a sibling with this most common form of glaucoma. However just because there is glaucoma in the family does not mean that a given individual will develop the disease.
- Higher than normal intracoular pressure. Generally pressures beyond 22 represent higher than normal pressures. While elevated pressure does not mean you have glaucoma, it is the single most important risk factor for the development of glaucoma. Therefore, elevated pressures, especially if combined with other risk factors, should be closely monitored.
- Race. An important risk factor for open-angle glaucoma, which is found to be four to five times greater in African Americans than in other races. Also, blindness from glaucoma is 4 to 8 times more common in African Americans than in Caucasian Americans. Asian-Americans seem more prone to develop angle-closure glaucoma.Other risk factors include:
- Diabetes
- Myopia (nearsightedness) Blunt injury to the eye
- Steroid medication use
- Hypertension
-
-
What’s the difference between a glaucoma suspect and a glaucoma patient?
Glaucoma can be extremely difficult to diagnose, particularly in the early stages. An example of a glaucoma suspect would be a person who may have elevated pressures, but a normal optic nerve exam and visual fields. Elevated pressure alone does not mean glaucoma, although it is an important risk factor (see question 5). Such a person would be monitored on an appropriate basis, and even perhaps treated if the pressure were high enough to be a significant risk.
-
How can I tell if I have glaucoma?
The vast majority of cases of early glaucoma have no symptoms. Except for acute forms of glaucoma, there generally is no pain or discomfort. Most patients are totally unaware that there is anything threatening their vision. In advanced glaucoma, patients may complain of generally blurred vision or loss of peripheral vision. In acute glaucoma, pain is prominent with other symptoms and signs such as red eye, halos, light sensitivity, and headache. The intensity of pain can vary from a low grade brow ache to intense aching.
The best method for diagnosing glaucoma is through a comprehensive examination. This should be done regardless of age, but especially if risk factors (Click here for more info) are present. Your ophthalmologist has a variety of diagnostic tools available in the investigation for possible glaucoma. Remember too that there are many other causes of blurred vision and ocular pain.
-
Is glaucoma painful?
Glaucoma is usually a painless disease. Pain is more related to the rate of pressure rise (as seen in the acute forms of glaucoma) and less related to the level of pressure itself. It is well known that high levels of pressure that occur slowly over a period of time have little or no symptoms of discomfort. We’ve seen patients with intraocular pressures of 50 millimeters of mercury (upper limits of normal – 22) and didn’t have a clue that anything was wrong. It is as though the eye acclimates and compensates. With sudden rises in pressure, however, discomfort may occur with pressures far below that level.
-
How is glaucoma diagnosed?
Most cases of glaucoma are “silent” meaning that there are no warning signs that
specifically point to glaucoma. Except in advanced cases where there may be profound visual loss, glaucoma generally goes undetected. An eye examination is the best method of glaucoma detection (see question 13 for details). During the course of an examination, if your ophthalmologist becomes suspicious of glaucoma, he may perform other tests to clarify
or stage the level of disease that a person may have. These tests are listed below:APPLANATION TONOMETRY
This test is a routine part of a complete eye examination. It is a painless method of measuring fluid pressure or intraocular pressure (IOP) of the eye, and is the preferred method used by Davidson Eye Associates. Elevated IOP is the single most important risk factor for glaucoma (Click here for details of risk factors). During this part of the examination, your ophthalmologist will put yellow numbing drops in the eye. (S)he will then shine
a blue light into the eye, while gently placing a measuring guage against the cornea to determine the pressure in the eye. This method is a highly accurate form of IOPdetermination and is completely painless.Applanation tonometry is the most common method of IOP determination. There are
other less common forms of pressure determination. For example, air puff tonometry reads IOP by blowing a puff of air against the eye. Because nothing touches the eye, numbing drops are not needed. Patients are aware of air being blown into the eye, however.GONIOSCOPY
This is a “non-routine” but extremely important test that allows examination of the angle
of the eye (see question 2 for details), and it is done only when there is suspicion of glaucoma or other problems. During this test, numbing drops are placed into the eye. The ophthalmologist will then gently lay a special lens against the eye that will allow visualization of the drainage channels and other structures located in the angle. This procedure is completely painless and takes only a minute or so to do in most cases.OPHTHALMOSCOPY
This is a normal part of a full eye examination where the optic nerve is examined under
high magnification. The optic nerve, color, circulation, and surrounding tissue can be evaluated for abnormalities (see question 2 for details).VISUAL FIELD ANALYSIS
This is a computerized analysis of the field of vision, and is the hallmark of glaucoma
detection and follow up. This test is extremely important because it can pick up early visual loss from glaucoma and can measure the degree of damage to your vision. Damage usually begins in the periphery (your side vision) where it is not noticed early on. In fact, loss
of central (straight-ahead) vision occurs late in the disease and usually after wide spread peripheral vision loss. This explains why glaucoma often goes undetected by the patient until
advanced disease occurs. This test also tracks whether your field loss is progressing or stabilized at its current level while under your doctor’s treatment plan.During this test, you will be seated in front of the visual field machine that your doctor uses.
Your head will be positioned before a white screen with your chin comfortably resting on a chin rest. Within this white screen will be a target that the testing eye (other eye will be covered) will fixate on. When the test begins, you will see spots of light of varying intensities flash one by one in different parts of your side vision. You simply press a button each time you happen to see a light stimulus. The computer then takes these responses and uses the information to form an analysis of your visual space. Sophisticated programs can
then compare your responses with what is statistically normal for someone your age and level of vision.The test is easy and is of course painless since it is a visual test. Testing programs have
become much more refined and do not take near the time or require
the concentration that programs in the past did.There are other tests that have become available for early glaucoma diagnosis, which concentrate on detecting early optic nerve disease. These technologies are still being developed and refined. They include the Heidelberg Retinal Tomograph, the GDx, and the Optical Coherence Tomography System.
-
What is the treatment for glaucoma?
Glaucoma is generally treated “medically” (observation in suspect cases, eye drops, and/or
rarely pills). Surgery (laser, traditional surgery) is generally reserved for cases that cannot be controlled medically. Some surgeons however are using laser treatment as the first line of treatment in an attempt to avoid daily use of eyedrops. Rarely in this country is a traditional
glaucoma operation performed before trying medical or laser treatment. Some countries however do traditional glaucoma surgery as their first line of treatment and claim good results. There are studies that are looking into which is the best initial treatment of glaucoma. Treatment however often includes a combination of methods.-
- EYE DROPS – In the USA, this generally represents the first line defense against glaucoma. Different drops, however, act differently upon the eye. Some lower intraocular pressure (IOP) by causing the eye to make less aqueous. Others help open up the drainage channels in the angle (see question 2 for details) to allow more fluid to exit the eye.
There are many types of eye drops used in glaucoma, and advances in pharmacology (the study of drugs) has greatly revolutionized the way glaucoma is treated. Depending upon the medication, drops may be used from once to four times per day, and may be used in combination with other drops.
All eye drops cause a certain level of stinging and burning, which should be very short-lived. Also, just like other medication, eye drops may uncommonly cause other side affects, such as blurred vision, redness, and even problems
such as insomnia, irritability, shortness or breath, heart rhythm disorders, and others. Your ophthalmologist should advise you of possible side affects of the drops that you’re on. Also,
make sure that (s)he knows what other medication you are taking. To minimize absorption into the bloodstream and maximize absorption into the eye, close your eyes for a minute or so and press against your tear ducts located in the nasal corners of your eyes. Your ophthalmologist can demonstrate proper eye drop technique for you.- LASER TREATMENT- See question 11
- TRADITIONAL SURGERY – See question 12
REMEMBER….
The goal of glaucoma treatment is preservation of long term vision. Attention to detail now will pay dividends later. Here’s what you can do:
- Always make sure you follow your doctor’s treatment plan. Have your
treatment plan written down if you have trouble remembering. - Always ask questions and be sure you understand your treatment.
- Always make sure that you understand your medications, doses, the timing
of administration, and their side effects. - Never under any circumstances change your medication dosing without
your doctor’s knowledge. MORE does not mean BETTER. - Always let your doctor know if you have difficulty remembering your
medicines and doses. Be sure to have your instructions written
down. - Always alert your doctor if you have persistent burning, redness, irritation,
or change in vision with your eye drops. - Always make sure your doctor knows if you have a change in lifestyle
habits. For example, if you work 1st shift on some weeks and
3rd shift on others, this may affect how you take your eye drops.
-
-
How does laser treatment work for glaucoma? Is the treatment painful?
When medication does not achieve the desired results, loses their effects, or is intolerable due to side affects, then your ophthalmologist may recommend laser treatment. There are basically two techniques of laser treatment used in the glaucomas. For acute glaucoma (Click here for more information), laser iridotomy is considered the treatment of choice after stabilization with medication. For open angle glaucoma and most other forms of chronic
glaucoma, laser trabeculoplasty is the technique of choice. See below for a description of both techniques.Laser Surgery
Davidson Eye Associates has nearly 20 years of experience with laser surgery for glaucoma. This treatment is highly effective for both acute and chronic forms of glaucoma.
At DavidsonEye Associates, laser treatment is performed in an office setting. Generally, patients come in an hour before the procedure to have some preparatory eye drops instilled. Just before the treatment begins, numbing drops are instilled which may cause short-lived stinging. During the laser procedure, patients will see bright flashes of light but will experience no pain otherwise. The procedure takes between ten and twenty minutes.
After the treatment, we will monitor the eye and its pressure for the first hour or two. Most patients can then resume their normal activities at home, although the vision in the treated eye may be blurred for several hours. There may be some minor discomfort for a few hours after the procedure. Initial follow up visit is then scheduled which can range from one day to one week after the treatment.
In acute glaucoma (Click here for details and pictures of a narrowangle), pressure can build up rapidly in the eye causing visually threatening damage to the optic nerve. In doing a laseriridotomy, an opening in the iris allows equalization of pressure in the posterior and anterior chambers. This allows pressure to flow directly into the angle for drainage, and also allows the peripheral iris to “fall back” or relax, creating a wider angle for better fluid flow. Laser iridotomy is generally curative in preventing attacks of acute glaucoma. For those who have suffered an attack of acute glaucoma, this technique can prevent further attacks but will not restore any vision that may have been lost.
For open angle glaucoma and other forms of nonacute glaucoma (click here for details), laser trabeculoplasty can be done to add control. Here, the laser beam heats up the trabecular meshwork causing it to “stretch open,” and allowing fluid to drain out more easily. In laser trabeculoplasty, approximately 80% of patients respond well enough to laser treatment to avoid surgery (see question 12). It may take several weeks to see the full effect, however. Although some patients find that the laser treatment allows control of their pressure without the use of eye drops, most find that eye drops at some level are still necessary. Remember, the goal of laser treatment is control of pressure, not the elimination of eye drops.
Laser surgery for glaucoma is generally considered a low risk operation, which is why it has become a common form of glaucoma treatment. An uncommon complication is a pressure spike which can usually be managed with medication and rarely necessitates mergency surgery. The risk for visual loss from pressure spike or mascular swelling is also rare. Laser surgery for glaucoma does not cause cataracts. ometimes laser treatment has no affect on the pressure. Even with successful treatment with a good pressure response, glaucoma must be monitored since the treatment can lose its effect over time.
-
When is surgery necessary for treatment of glaucoma?
In this country, surgery is considered as a last resort when other treatments such as medication and laser surgery have failed. There are several types of glaucoma operations performed world-wide. The most common performed procedure, however, is called a trabeculectomy. This surgery involves removing a portion of the trabecular meshwork (Click here for details) which allows the aqueous to drain out of the eye more easily resulting in lower intraocular pressure (IOP).
Glaucoma surgery is generally done as an outpatient procedure under local anesthesia with sedation. Unless there are complications, patients go home an hour or so after their surgery. Patients are seen the next day for a post-surgical evaluation of the eye, vision, and for measurement of the IOP. It can take several weeks for vision to get back to its baseline following the operation. Postoperative medications generally include an antibiotic drop, an anti-inflammatory drop, and a cycloplegic drop (keeps the pupil dilated and helps manage pain). Glaucoma drops may be continued at some level depending upon what your ophthalmologist feels is needed.
The postoperative period generally lasts two to three months. The majority of patients do well with surgery, and most find that surgery controls them without the use of medication. There are risks to the procedure, especially in advanced glaucoma. Risks can include visual loss, cataract development from the procedure, or a failed procedure necessitating a re-operation.
-
How often should I have my eyes examined for glaucoma?
Routine eye examinations are a vital part of maintaining ocular health and detecting silent disease. Recommendations for eye examinations vary. For the detection of glaucoma, Davidson Eye Associates recommends the following schedule as a guideline. Precisely how often a patient should be seen will depend upon their circumstances and risk factors.
Davidson Eye Associates Recommended Guidelines
NO RISKFACTORSRISK FACTORSUnder
30 yrs ageEvery
4 yearsEvery 6 months
to 2 years*30
– 45 yrs ageEvery
2 – 4 yearsEvery 6 months
to 2 years*Over
45 yrs ageEvery
1 – 2 yearsEvery 6 months
to 2 years*Risk Factors
- Age
- Family History
- Elevated IOP
- Race
- Diabetes
- Hypertension
- Blunt Injury
- Prolonged use of steroid medication
*Note: Recommendation depends upon the type and number of risk factors involved. Click here for details.
-
Is there a video I can watch that explains Glaucoma?
Here you go!
